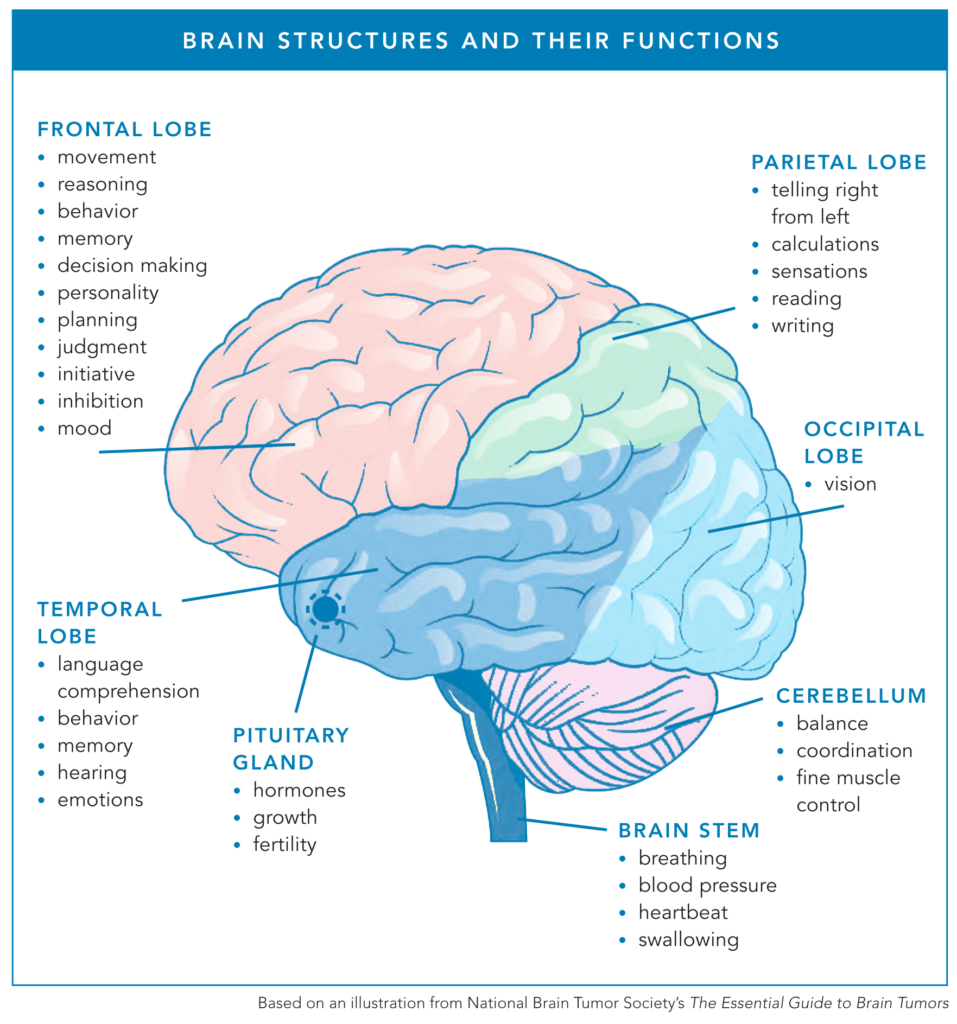
Today, nearly 1 million Americans are estimated to be living with a brain tumor. Depending on their tumor’s location, some patients with brain tumors face ongoing speech and language challenges, including difficulty speaking, finding words, and slurred speech.
“If your tumor is in one of the temporal or parietal areas that affect speech, you might be able to walk, but you might not be able to get your words out,” neuro ICU nurse Stacy Bournousouzis shared.
Speech language pathologists (SLPs) can play an important role in supporting patients with brain tumors at nearly every step of their brain tumor experience.
Speech vs. Language
SLPs are specialists trained to help patients with speech and/or language challenges.
A patient who wakes up from brain surgery with one-sided facial paralysis or hemiplegia may experience difficulties with speech, so an SLP might evaluate and treat the patient to help retrain facial muscles. The same SLP would support a patient with aphasia in a different way, as they need language support.
Speech
Therapists help to improve the way speech sounds by focusing on how articulators — one’s lips, teeth, mouth, and tongue — and muscles create clear speech that can be understood.
Examples of speech challenges that some patients with brain tumors may face include dysarthria and apraxia of speech. Dysarthria can cause slurred speech due to muscle weakness, making it hard to pronounce words, whereas apraxia is a challenge with motor speech planning.
“With apraxia, you know what you want to say, but it just doesn’t come out,” said Christina E., who was diagnosed with anaplastic astrocytoma (grade 3) in 2016 while doing her pre-doctoral internship in clinical psychology. Side effects from radiation after a glioblastoma diagnosis three years later caused speech difficulties for Christina.
Language
Language refers to how people select words, use grammar, put thoughts together to convey them to others, and understand what others say. Language includes oral communication like a spoken conversation as well as reading, writing, texting, or typing.
A common language difficulty for patients with brain tumors is called aphasia, when a person has difficulty understanding or expressing oral language due to damage to a part of their brain responsible for language.
“Aphasia is when you’ve lost your train of thought, or you can’t think of the word,” said Joseph, Christina’s husband. “It’s just not there. Because of this language difficulty with aphasia and apraxia of speech, Christina has been unable to work as a psychologist wherein communication between client and therapist is vital.”
There are quite a few different types of aphasia, which can be influenced by the location of the brain tumor. For patients like Matt D. with expressive aphasia, also known as Broca’s aphasia, the difficulty is found in how they express themselves verbally. They know what they want to say but struggle to find the words to articulate their thoughts.
“I first had expressive aphasia 9 and a half years ago,” Matt said. “Then I had a hemorrhage three years ago, and then the expressive aphasia was even worse where I lost my ability to have imagination. It just completely changed how I viewed things.”
Difficulties Communicating with Others
Whether it’s because of the tumor, surgery, or side effects from treatment, patients with brain tumors can face difficulties trying to communicate with other people.
“The kind of work we do is based on functional communication, whether that’s at work or just communicating with people at home,” explained Sarah Steele, MS, CCC-SLP, of the Massachusetts General Hospital (MGH) SLP Brain Tumor Team. “I think that’s where we find that people express the most frustration. People don’t understand that it’s like an invisible injury – that invisible cognitive or language change. A lot of patients mentioned when their hair grows back over their surgery scar, and it’s not as noticeable to others anymore, that people are not as patient with them anymore. They don’t give them the time because it’s not as apparent that they’re having some of the challenges that they have. A little bit of self-advocacy can help manage those situations.”
What can patients do to help ease communication challenges?
Let the people in your life know how you would like to be supported when you are struggling with issues like word finding. Some patients will want to push through and get the satisfaction of finding that word. Other individuals may prefer a simpler outcome where they welcome someone to jump in and help.
“It’s a conversation that’s worth having,” said Nate Somes, MS, CCC-SLP, of the MGH SLP Brain Tumor Team. “I think a lot of times people don’t know how to talk about those things, so that’s something we try to facilitate.”
If you find that you’re in a conversation with someone, and they are talking about a topic that you don’t engage with often and makes word-finding more difficult, try to talk about the topic more often.
“The frequency of the words you’re looking for, how often you get exposed to them, or how often you might use them really matters,” said Amy Maguire, MS, CCC-SLP, of the MGH SLP Brain Tumor Team. “The frequency of the word and the ease of retrieving it are related. If we want to improve naming or word finding, sometimes we just have to keep talking about these topics a lot more than we expect to help move things along.”
With aphasia, for example, it can be helpful to talk about other meaningful associations and boost one’s vocabulary around the topic.
“If we’re talking about coffee, we might also activate mug, beans, or something else that’s meaningful, like milk,” Amy said. “We want to associate all those things and activate that whole meaningful network to have a better shot at accessing the word. It can be really useful to enrich the conversation with other related words.”
The act of getting stuck can become an issue of its own. The automatic reaction when you can’t find a word is just to buckle down and stop at nothing to find it.
“That can be a counterproductive effort a lot of times,” Nate said. “Not only does it make it less likely to find that word, but it can derail the whole train of thought that you had going. It can be very helpful to work on releasing that moment, acknowledging it, and trying to scoot around it in some way.”
When struggling to find a word, you can try to paraphrase the target word. For example, you may not be able to recall the word car, but you could try to say “the thing that you drive in” or say a synonym like “vehicle.”
“I have several patients who like to use the not-this phrase,” Sarah shared. Continuing with this example, you could say, “It’s not a boat, but it goes on land.”
“If you have apraxia of speech, it’s going to be really important to take your time when you speak and to try to hear the words that you think you’re trying to say very loudly and almost visualize what the lip shapes would be on someone else,” Amy explained. “It’s about trying to activate the right motor planning instructions.”
What can care partners and other individuals do to help ease speech and language challenges?
“One of the things that I frequently encourage people to practice is how you repeat information for your loved one in a way that isn’t pedantic,” Nate explained. “How do we get to more naturalistic repetitions in conversation? How can I basically say the same thing twice without saying it like, ‘I’m telling you again.’ That can be really helpful because it starts to build a habit.”
It gives the patient, who is experiencing this language change, one more opportunity to get the information and helps slow down the pace of the conversation in a very supportive and relevant way.
“My brain can’t really keep up with the conversations,” Matt explained. “I have to slow down with everything, but that requires someone else to try to slow down as well and finally be on the same page, which can be challenging.”
“That’s one thing I would recommend to people if their partner, spouse, or friend — whoever is newly diagnosed with a speech impairment — feel it out, but let them finish their thoughts,” Joseph shared. “If they want you to interject, then they’ll prompt you. You just have to feel it out together. Some just hate it, but some want the help.”
If the patient is comfortable with more support, it can be helpful to say, “Don’t worry about it. I know what you meant.” This comment can help convey the larger message without putting pressure on them to find the word.
If the patient is open to some support, it can be helpful to suggest options for them to choose from. For example, “Did you mean car or vehicle?”
However, some patients want their communication partners to refrain from jumping in. Christina used to want help but later asked her husband Joseph to be patient and let her finish her thought.
As a mother to a child diagnosed with DIPG, Mia M. researched the typical progression of the disease to find ways to navigate future symptoms.
“I felt that if I knew enough to be able to acknowledge and understand the symptoms that were coming, then I would be better prepared,” Mia said. “For example, I knew he wasn’t going to be able to speak again. So knowing that ahead of time, I would think in what ways can we start acting now to make it easier for us to communicate with him.”
People communicate nonverbally, so we can pick up on many cues and find their meaning even if the words aren’t perfect. Examples of nonverbal communication include hand gestures, pointing to pictures, or even writing what they want to say.
While speaking with your loved one in ideal conditions won’t always be possible, you can certainly find ways to ease their difficulties.
- Speak in shorter, simple sentences to increase their ability to process information faster.
- Minimize distracting background noise to help the patient hold their attention longer (e.g., turn off the TV or music in the background).
- Avoid talking loudly or talking down to them like a child. It is important to keep a respectful and conversational tone as much as possible.
- Increase your use of hand gestures and other nonverbal communication to make it easier for them to follow along.
- Ask questions that can be answered by a simple yes or no instead of relying on open-ended questions.
- Avoid quickly switching topics within a conversation, as that can be more challenging to follow along.
A Final Reminder
A patient’s speech and language can change throughout their brain tumor experience. It can be a frustrating process that ebbs and flows over time. With that in mind, focus on the most beneficial approach in your current circumstances, knowing that you can change your course of action as your situation changes.