Radiation therapy is a common type of brain tumor treatment. If you’re feeling nervous, you’re not alone. These tips from patients and caregivers can help you feel more prepared before your first radiation session.
The content in this blog post is for informational and educational purposes only. It does not constitute medical advice. Please speak with your health care team to discuss your particular circumstances before making any decisions.
Tips to Consider Before Radiation
There are several steps you can take before your first radiation therapy session to feel more prepared.
1. Understand the Process Ahead of Time
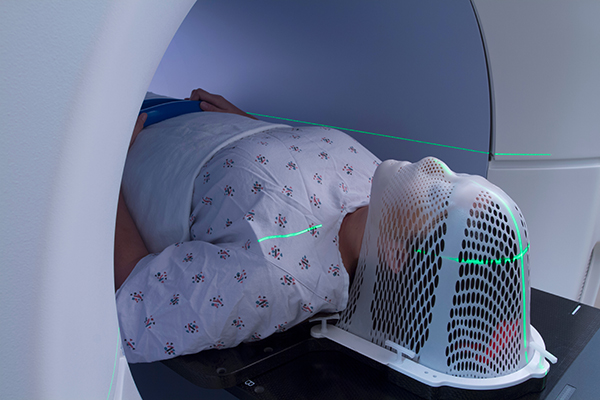
Understanding the steps involved in radiation therapy — like simulation scans and face mask fitting — can reduce fear of the unknown. Reading about what to expect and watching short videos about the process can go a long way in making your experience feel less overwhelming.
“While my technician did everything he could to put me at ease, the entire process caused me terrible anxiety,” said Barbara T., who has CNS lymphoma. “I think it would have helped me to see a video of the [mask-fitting] process ahead of time, as I was already overwhelmed from the diagnosis.”
2. Bring Questions to Your Initial Appointment
Your first meeting with your radiation oncologist is a great opportunity to ask questions and express any concerns you may have. Anxious about feeling claustrophobic? Ask about how they can help. Writing your questions down ahead of time on paper or a note-taking app on your phone can help ensure you don’t forget something important when you meet with your doctor.
Need help getting started? NBTS has drafted key questions you may want to ask during this appointment.
3. Make a Transportation Plan
Radiation therapy typically happens five days a week over about 30 sessions, and transportation can be a major challenge, especially if fatigue becomes a factor. Some patients can drive themselves, but many rely on others for rides. Care coordination apps or a spreadsheet can help you or your caregiver manage your rides, childcare coverage, and backup plans during radiation.
“Radiation takes a village,” said Stacy P., a neuro ICU nurse and a grade 3 astrocytoma survivor. “I realized that because it’s five days a week for me personally. A lot of the time, you have to make your plan with your doctor, and then you have to make your plan with your supporters because you can’t do it by yourself.”
As you consider who can take you to your appointments, think about whether someone needs to stay at home and care for your children.
Holly G., who received radiation therapy for grade 3 astrocytoma, set up a schedule with a consistent driver each day of the week.
“My husband, Matt, took me to radiation on Mondays through Wednesdays, my girlfriend Heather took me on Thursdays, and my sister took me on Fridays,” Holly shared. “Matt would stay home with the kids on Thursdays and Fridays. When Matt took me to radiation, my girlfriends or family would come and watch the little ones.”
Having trouble securing transportation? Discuss possible free or discounted resources available through the hospital or local nonprofits with your social worker. For example, the American Cancer Society’s Road to Recovery program offers free rides to cancer-related medical appointments.
4. Pick Appointment Times That Work for You
Once you’ve determined your transportation, discuss with your care team scheduling your daily appointments at a time that suits your routine.
Some patients prefer going early to get it over with or because it works better for their driver, while others schedule later in the day to accommodate work or family responsibilities.
“I made sure to schedule my treatments in the afternoon when my work day was done and after I had eaten lunch,” said Sara P., who received radiation for meningioma. “I did not want the fatigue to affect my daily work routine.”
Ask if your treatment center allows you to pick a consistent time slot to help with your planning.
Tips to Consider for Mask Fitting
Some patients describe the experience of getting fitted for a mask as almost therapeutic, while those with claustrophobia may struggle with the mask-fitting process. In addition to watching a video of the process ahead of time, as described in tip #2 above, there are other ways to support yourself.
5. Close Your Eyes
The most common tip we received was encouraging people to close their eyes during the mask fitting.
“I highly recommend closing your eyes and focusing on your breathing while they’re fitting the mask,” said Kendra L., who was treated for hemangioblastoma. “The mask has holes in it so you can see light, but it’s very close to your face and can give a sense of claustrophobia in a way. I just found it easier to close my eyes.”
6. Practice Meditation and Mindfulness
If you’re feeling anxious about your mask fitting, turn to meditation and mindfulness exercises to help you relax.
“Getting yourself in a good mindset and some breathing exercises really helped me through the mask fitting,” said Joe M., who has grade 4 astrocytoma with IDH mutation. “I think a calm mindset is the best way to approach it.”
You may find comfort in reciting affirmations, mantras, or religious texts. You can recite these phrases mentally during the mask fitting, especially if there is a particular phrase that you find empowering.
“There are tons of mantras, affirmations, and prayers that you can choose from,” said Victoria B., who cared for her mother with glioblastoma. “Find the words that mean the most to you. One I use often is reminding myself repeatedly that ‘I can do hard things.’”
7. Use Creativity with Pediatric Patients
For pediatric patients, treatment teams often take extra steps to make the mask-fitting experience less intimidating. Ask your child’s team if they can decorate the mask, giving it a superhero or fantasy theme.
“My son was 15 [when he was diagnosed with a brain tumor],” Julie K. said. “They decorated the mask like Spider-Man since he loved Spider-Man as a kid.”
Kathryn D. leaned into calling the proton radiation room a “spaceship” to help her almost 3-year-old son, who had been diagnosed with grade 3 supratentorial ependymoma, associate the experience with something positive.
“He would ask each day if he was going to ride the spaceship today,” Kathryn shared. “We tried to make the experience as fun as possible for him. For his final treatment, we dressed him in an astronaut costume. It made everyone’s day!”
8. Relax Your Body
Relaxing your body, particularly your face and shoulders, will make for a more comfortable mask during your future radiation sessions.
“Try to relax your face during the fitting process,” said Tim P., who received radiation for meningioma. “If you clench, the mask will only feel tighter once it dries and hardens for treatment. This happened to me the second time I had Gamma Knife, and it was notably more uncomfortable during treatment.”
9. Consider Shaving Facial Hair
Even if your treatment center does not require patients to be clean-shaven, you may find it more comfortable to be fitted for your mask without any facial hair.
“After my surgery and during my treatments, I decided to let my beard grow out,” said Michael B., a firefighter who was diagnosed with oligodendroglioma. “I had a good start on a beard when I went in for my mask. When they put the hot plastic on my face to form the mask, it was warm but not overly uncomfortable. It wasn’t until the mask cooled off and it was time to remove it from my face that there was some pain. The plastic cooled and stuck to the hair on my face. The tech tried to be careful, but there was no way to take it off without pulling hair out. We did have a good laugh after that.”
Once the mask is fitted, it is recommended not to make changes to your facial hair or hairstyle, as these can affect how the mask fits.
Next Up: Tips for Navigating Radiation
In part three of our radiation therapy series, we’ll share tips from patients and caregivers on navigating daily radiation therapy sessions.