Each year, more than 39,000 Americans are diagnosed with meningioma — the most common type of primary brain tumor. Meningiomas originate from cells of the meninges, which are membrane layers that cover and protect the brain and spinal cord.
While often benign, these tumors can still cause serious health issues depending on their size and location. Let’s talk about what makes meningiomas different from other brain tumors and learn more about the experiences people living with this tumor type and their loved ones may face.
Grades of Meningioma
Meningiomas can be benign (grade 1), atypical (grade 2), or malignant (grade 3). Treatment and prognoses vary between meningioma grades.
Grade 1 meningiomas are the most common, accounting for 41.4% of all brain tumors and 56.8% of all non-malignant brain tumors, according to CBTRUS.
“Grade 1 meningiomas are thankfully the most common and least aggressive,” said Keck School of Medicine of USC neurosurgeon Aaron Cohen-Gadol, MD. “If somebody is unfortunately suffering from a grade 1 meningioma and they undergo surgery by an experienced surgeon, the outlook and prognosis are excellent.”
Some patients with slow-growing grade 1 meningiomas experience minimal symptoms after their craniotomy.
Alan S. said, “Multiple preparatory tests, office visits, a 13-hour surgical procedure, three days of hospital intensive care, and recovery guidance for the long term all contributed to the successful eradication of, and recovery from, a benign 4.8 cm meningioma brain tumor. I am so fortunate to be living a normal life as if it never occurred!”
Atypical (grade 2) meningiomas are less common than grade 1 meningiomas.
“Atypical meningiomas have intermediate characteristics between benign and malignant grade 3 tumors,” Dr. Cohen-Gadol (Cohen) said. “They tend to grow faster than grade 1 tumors. Atypical meningiomas have some cellular features — increased cell division and a typical cellular appearance — under the microscope that suggest they could become more aggressive.”
These tumors also have a higher chance of recurrence, especially if surgeons are unable to remove the entire tumor.
Grade 3, or malignant, meningiomas are the rarest and most aggressive. They account for just 0.3% of all brain tumors diagnosed each year, according to CBTRUS.
The National Cancer Institute reports that an estimated 3,360 people are currently living with high-grade meningioma.
“Grade 3 meningiomas are aggressive tumors that can grow quickly and have a high tendency to invade surrounding brain tissues,” Dr. Cohen said. “Their removal is difficult because of the infiltration of normal tissues.”
Although rare, they can even spread to other parts of the body. These tumors are more likely to return after treatment and are less responsive to therapy than lower-grade meningiomas. Treatment involves surgery, radiation therapy, and sometimes chemo, but grade 3 meningiomas are less responsive to treatment than lower-grade meningiomas.
The Role of the NF2 Gene
Some meningiomas are associated with a genetic condition called neurofibromatosis type 2 (NF2). People with NF2 are more likely to develop multiple brain tumors, including meningiomas and vestibular schwannomas, due to mutations of the NF2 gene, which normally helps control cell growth. When this tumor suppressor gene isn’t working properly, it can lead to tumor development.
Research published in the International Journal of Molecular Sciences found that 50-60% of meningiomas involve either an inactivating NF2 mutation or loss of chromosome 22, where the gene is located.
Knowing whether a tumor has an NF2 gene mutation can help patients and their providers make informed decisions about their care. That’s why understanding the tumor’s biomarkers is so important and why NBTS launched MyTumorID to help raise awareness about the importance of biomarker testing for people with brain tumors.
In patients with NF2, meningiomas are often more aggressive. Another International Journal of Molecular Sciences article notes that 50-75% of people with NF2 develop meningiomas, which are more likely to be grade 2 or 3. These meningiomas have a worse prognosis and higher recurrence rate than sporadic meningiomas.
Surgery
Not every meningioma requires immediate surgery, but for many, it’s the first line of treatment.
“Small [meningioma] tumors that are asymptomatic, especially in older patients who may not tolerate a surgery very easily, can be watched,” Dr. Cohen said. “Tumors that are large and causing symptoms, especially in young individuals, should be removed. Large tumors in young individuals, even though they may not have a lot of symptoms, may be removed because these tumors tend to grow slowly, but they still grow.”
There are key factors that determine how aggressively a neurosurgeon can remove a tumor, including its location and size. According to UCLA, “up to 85% of meningiomas are curable with surgery” for tumors in favorable locations.
“The surgeon’s experience and technique are also important,” Dr. Cohen said. “Experienced surgeons can provide a much more effective resection. Surgeons who have been doing this for a long time can be effective in removing almost all of the tumor.”
National Brain Tumor Society encourages patients to seek a second opinion before surgery when it’s safe to do so.
“I think second opinions are very important,” Dr. Cohen said. “Surgeons who specialize in the removal of meningiomas tend to have better outcomes and can remove an additional portion of the tumor safely. That can really affect the lifespan of the patient. Your health is your most important asset. Therefore, you should get the best surgeon to take care of you.”
Radiation
Radiation therapy may be recommended when full surgical removal isn’t possible, when the tumor is located near sensitive brain structures, or in the event of recurrence.
“The neurosurgeon got as much out as he possibly, but we knew that he didn’t get it all,” said Tim P., who was diagnosed with a softball-sized meningioma. “I didn’t understand how common it is for my type of tumor (atypical meningioma) to recur. Two years after surgery, my semi-annual scan showed a recurrence, and I was told I needed to do radiation to try to prevent further growth.”
Radiation may be done as traditional radiation, proton radiation, or stereotactic radiosurgery. According to UCLA, “stereotactic radiosurgery stops the growth of meningiomas in up to 80% of cases.”
“We spent a week at Mayo, meeting with several different neurosurgeons and radiation oncologists,” said Amanda B. “Ultimately, they said the same thing. My tumor wasn’t in a location that they wanted to operate on because it was near my cranial nerves and my carotid artery. I was not a candidate for fractionated radiation, but I was a candidate for Gamma Knife radiation (a type of stereotactic radiosurgery).”
Precision Medicine
NBTS is funding a research project to explore the potential of precision medicine approaches for certain types of malignant meningioma. This drug combination has demonstrated decreased tumor growth in laboratory models of meningioma. Pending positive results from this study, plans are in place for rapid translation of this combination into the clinic in partnership with Alliance for Clinical Trials in Oncology.
Common Meningioma Symptoms & Side Effects
As with any brain tumor, symptoms and side effects vary depending on the tumor’s location and size.
“The location of the tumor is critical not only for the symptoms but also for how easy it is to remove it completely,” Dr. Cohen said. “If it’s engulfing critical structures, we have to leave some of the tumor behind to protect important functions.”
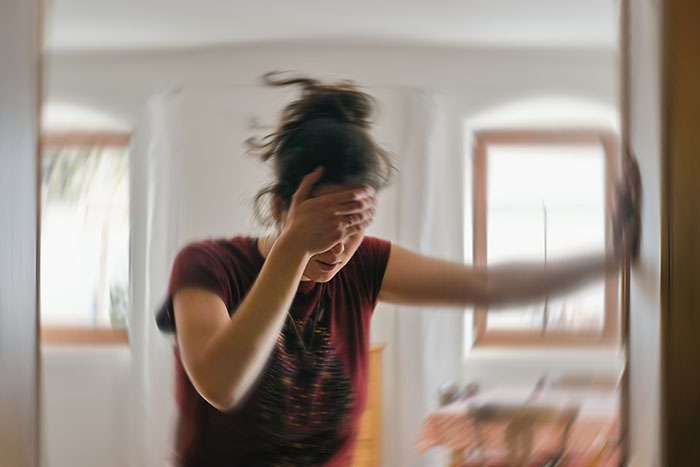
Symptoms of a meningioma tumor may include:
- Persistent headaches
- Seizures
- Vision problems
- Cognitive challenges
- Personality changes
- Balance or coordination difficulties
- Weakness or numbness
- Hearing loss or ringing in the ears
- Nausea and vomiting
- Sensory changes, such as tingling pins and needles
“Headaches are often described as persistent or unusual because the tumors can press against the brain or skull and cause increased pressure,” Dr. Cohen said. “Please remember that most people who have headaches do not have a tumor. If the headaches are persistent or considered unusual, then obviously that raises the suspicion of the presence of a tumor.”
Following surgical resection, some patients experience minimal symptoms.
“Day to day, it doesn’t impact my life,” Tim shared. “If anything, it’s helped me in ways, just to become a little bit more determined to achieve a healthier lifestyle.”
Other patients with meningioma face longer-term symptoms and/or side effects from treatment.
Seizures
More than one-third of people with meningioma will experience seizures at some point. An article in Neuro-Oncology Advances estimates that 10-50% of patients may have seizures that significantly impact their quality of life.
“As meningiomas grow, they can interfere with electrical activity and irritate the surface of the brain, leading to seizures, especially if the tumor is located in the parts of the brain controlling motor movement of the arms and legs,” Dr. Cohen said.
Some patients experience generalized seizures, which impact both sides of the brain, while others have focal seizures, which happen in only one part of the brain, so they can be harder to detect.
“I thought a seizure was collapsing, convulsing, and possibly losing consciousness,” said Erica R., who was diagnosed with meningioma in her right temporal lobe. “When I would have a seizure, I would first get an overwhelming feeling of fear. Then I felt as though I was leaving my body. I had a feeling of déjà vu, nausea, felt as if I was losing control of my bladder (I never did), I would get hot, and my heart would beat very fast. I had all of these symptoms at the same time. The feeling was scary, and although I knew it would be over in less than 15 seconds, it felt like a lifetime.”
For some, seizures can persist even after treatment. According to Frontiers in Oncology, around 12-19% of patients continue to have seizures following surgical removal of their tumor.
Vision Changes
When meningiomas grow near the optic nerve or visual pathway, they can lead to vision problems, including double vision, blurred vision, or loss of peripheral vision.
“I have a meningioma tumor behind my left eye,” said Carrie E. “I probably would have never known that I had it, except for the fact that it caused pressure behind my eye and made it bulge. My vision also started getting worse in that eye, which was why I initially went to an ophthalmologist.”
For some, vision changes may seem temporary or unrelated at first.
“I was in Las Vegas with a group of friends, and noticed I was seeing double when I woke up in the morning,” Tim said. “I chalked it up to a couple of late nights, but I continued to see double for four straight days. It just wouldn’t go away.”
In some cases, vision loss can be permanent, whether caused by the tumor itself or treatment side effects.
“I lost the vision in my right eye due to damage to three of my cranial nerves during radiation,” Amanda said. “My eyelid doesn’t open anymore — it just stays closed, and it will never fix itself. You feel like you’re losing so much.”
Cognitive Challenges
Meningiomas can cause cognitive changes, especially when they grow large or are located in the frontal lobes — the part of the brain responsible for decision-making, memory, attention, executive function, and emotional regulation.
Symptoms may include difficulty concentrating, memory problems, confusion, speech difficulties, or even personality changes. Studies have linked meningiomas to impairments in working memory, processing speed, verbal fluency, and other cognitive domains.
For many patients, these challenges can be life-altering.
“I still face many challenges — fatigue, memory, concentration, and other surgery-related issues — so I was unable to return to my executive marketing position in January 2025,” Beth E said. “The company could no longer hold my job, so after 33 years, I am officially retired. I was not prepared emotionally or financially to retire, so it’s been difficult to move forward.”
Even years after treatment, many patients continue to adjust to a new normal — one that can come with lasting cognitive hurdles.
“Six years later, I suffer from some short-term memory loss, speech aphasia, and trouble with numbers,” said Annie M. “But I’m grateful to be alive!”
Returning to work or navigating daily conversations can be especially difficult when word-finding issues arise.
“I’ve improved with word finding, but I haven’t been able to get back to my old self,” said Chaka C. “I’m afraid of saying the wrong word. What if it’s not the right word, or I say it wrong?”
Benign is Not Fine
A common refrain among people living with meningioma is that “benign is not fine.” While a majority of meningiomas are non-cancerous, that doesn’t mean the experience is easy.
“My treatment was the same as it would be for someone with brain cancer — same radiation, same recovery,” Amanda said. “And still, people say things like, ‘It’s not cancer, why are you upset?’ Everything in your brain is vital for your function, so anything that’s in there, taking up space and pushing on your brain tissue that’s not supposed to be in there is bad.”
Even well-meaning comments like “you look great” can diminish a difficult reality.
“Every comment minimized what I went through,” said Heather O., who spent 17 days in the ICU and had to relearn how to walk and talk.
What Not to Say: “At least it’s not cancer. You’re so lucky.”
What to Say: “I’m sorry to hear about the challenges you’re experiencing.”
“Some people don’t think about what they say,” said Erica R. “My experience is life-altering. I lost sleep and weight, and I was consumed by this diagnosis. Post-surgery, I was affected by bright lighting and crowds at times. It was harder to concentrate. I was impatient with myself. I wish I hadn’t been so much. I had an 8-hour craniotomy. I had my brain manipulated, a lime-sized tumor removed from the meninges of my outer brain, and seizure activity, so I was unable to drive for months due to this. I lost some of my independence.”
The physical and emotional toll can be long-lasting: vision loss, seizures, cognitive and speech difficulties, job loss, and identity changes.
“It’s a lifelong battle,” Tim said. “I have scanxiety — every scan, I’m definitely a bit on edge. Those results are always bringing a certain level of anxiety, and I wonder about whether or not there has been another recurrence.”
Even if the patient doesn’t have any lingering symptoms, survivor’s guilt can take its toll.
“After a 5-week recovery, I returned to work both times,” said Karen K., who had two craniotomies to address meningioma tumors. “I looked the same. I acted the same. I was running 12 miles a weekend. Opening a business. If I didn’t tell you, you’d have no idea seven silent monsters used to live in my head. That is both a blessing and a curse. But where do I fit in? I joined this community of brain tumor survivors, but I didn’t feel worthy. I bounced back, but the mental and emotional toll on myself and my husband has been more lengthy.”
Navigating Work
Returning to work after surgery or radiation looks different for everyone with a meningioma. Some people are able to return after a short recovery, while others require more time or to make longer-term adjustments.
“I took short-term disability and returned to work after about six weeks,” Tim said. “There were days I felt ready to jump back into normal routines, but I had to balance that with the reality of my brain needing rest. Even a desk job can be mentally exhausting in recovery.”
For others, returning to the same role isn’t always possible. Some patients change careers or reduce hours.
“I couldn’t go back to my job as an educator,” said Nakeisha C. “I actually had to change careers to be in a safer work environment.”
Leaving a job not only brings about a significant change in one’s daily routine, but it can also impact one’s identity and sense of purpose.
“I’m planning to take two years to focus on my healing, but it’s hard because I’ve always worked,” said Stephanie L., who worked as a nurse at the time of diagnosis. “Unfortunately, in our society, we tie that to identity, so it’s hard for me to be in a room and not have those titles, but those things come and go. Yes, my meningioma was benign, but it still has a significant impact on my life. I think that’s the important part for people to understand. Post-craniotomy, it’s a new you.”
Financial Hardships
The financial burden of a meningioma diagnosis can be significant. Even with insurance, the costs of surgery, treatment, follow-up scans, medications, and missed work can quickly add up, especially for those who need to temporarily or permanently step away from their jobs.
“I’m really thankful that my insurance company was able to cover my brain surgery because it was over $200,000 for everything,” Tim said.
For others, financial strain can lead to difficult decisions and the need to lean on community support.
“I did consider stopping the infusions because of the cost,” Amanda said. “At first, I was completely against starting a GoFundMe. I didn’t want to ask for help. But the bills kept piling up, and we still had three kids at home. I had to swallow my pride. It’s amazing what people will come together to do.”
Amanda also worked closely with her medical center’s financial counselor to pay her medical expenses.
“Mayo Clinic helped me set up a payment plan with no interest,” Amanda said. “I got to choose the amount and how long I wanted to pay it off.”