What if we could flip one of glioblastoma’s biggest strengths — its resistance to treatment — into a targetable weakness?
That’s exactly the idea behind a new treatment strategy developed at UCLA – based on research NBTS helped fund – which is now moving out of the lab and into a newly opened clinical trial for patients with recurrent glioblastoma.
Why glioblastoma is so hard to kill
No matter how aggressively doctors treat it, glioblastoma seems to always find a way to come back. And despite the intense focus and urgency surrounding glioblastoma research, this tumor remains one of the most stubbornly lethal cancers in all of medicine.
A key reason? These tumors are hardwired to resist treatment by blocking the natural process of cell death – a built-in defense system that protects our bodies – but, when hijacked by cancer, becomes one of its greatest weapons.
When a healthy cell is damaged beyond repair, it typically goes through a process that helps the body remove it. Scientists call this process apoptosis, or programmed cell death. Think of it as a “self-destruct” mechanism that protects us by eliminating malfunctioning cells.
Most cancer therapies rely on this process. Treatments like radiation, chemotherapy, and targeted drugs all aim to trigger cell death in tumors.
But glioblastoma tumors are notoriously good at blocking these self-destruct signals. These tumors have evolved ways to block the cell’s death signals — allowing them to survive even after the most aggressive treatment. If the cells won’t die, the tumor won’t go away.
Understanding how glioblastoma prevents apoptosis is a major focus of research in the field.
That’s the core challenge a team of UCLA researchers — Drs. David Nathanson, Tim Cloughesy, and Elizabeth Fernandez — set out to solve, with support from NBTS. They wanted to know: How exactly is glioblastoma stopping cell death? And could that very mechanism be used against it?
Finding the tumor’s “shields” & learning how to breakdown these defenses
The team studied more than 50 glioblastoma tumor samples that had been grown in the lab from real patients’ tumors — what scientists call patient-derived tumor models. These models closely mimic how the cancer behaves in the body, making them a powerful tool for research.
Using two powerful techniques — genetic sequencing and functional testing — the team mapped out how these tumors resist therapy. Genetic sequencing identifies which mutations and features were present in each tumor’s DNA, and functional testing observes how those tumors responded to different treatment conditions in real time.
By combining these tools, the team was able to map out how glioblastoma tumors protect themselves from treatment — and identify a weak spot that could be used to shut down those defenses and trigger cell death.
“Many cancer treatments are based on the genetic profile of a patient’s tumor,” said Dr. Nathanson. “However, genomic features alone can’t always predict how a tumor will respond to a therapy. This study explores a new approach that looks beyond the tumor’s genetic blueprint, in which we combine genetic data with functional tests to show how live cancer cells respond to treatments. This gives us a much clearer picture of what treatments will work and why.”
They found that nearly all glioblastoma tumors rely on two proteins to stay alive: MCL-1 and BCL-XL. These proteins act like shields, helping tumors block treatment signals that normally trigger cell death. This system of two lines of defense is a major reason glioblastoma has been so difficult to treat.
Yet, what the UCLA team discovered is that in many glioblastoma cases — especially those without changes to a gene called p53 — standard therapies like radiation or chemotherapy already weaken one of those shields: MCL-1.
That leaves the tumor dependent on BCL-XL for survival. If researchers can remove this last line of defense when the first block (MCL-1) is already gone, they may be able to finally get the tumor to die through apoptosis.
This idea — using one treatment to expose a vulnerability, then another to exploit it — is known as synthetic lethality. And it’s becoming one of the most intriguing concepts in cancer research.
A new precision weapon: delivering treatment directly to the tumor
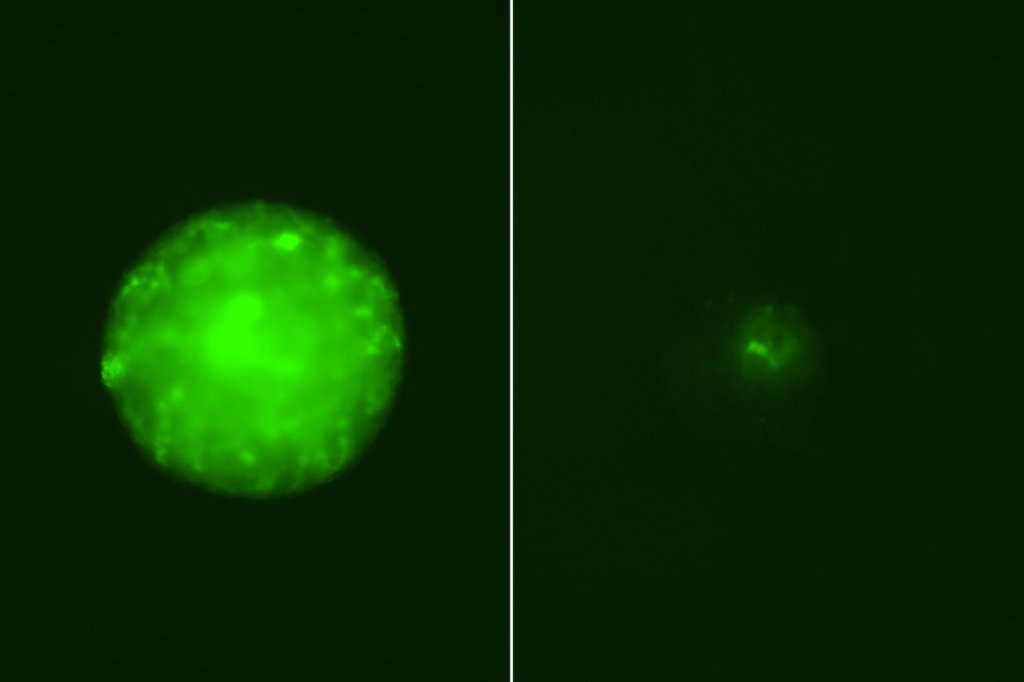
Targeting BCL-XL is tricky. A drug called Navitoclax tried it before — and worked — but it also caused serious side effects by hitting healthy cells.
So, the UCLA team worked with researchers at AbbVie to test a smarter approach: antibody-drug conjugates (ADCs). These are a promising class of precision drugs that use a tumor-seeking antibody — like a guided missile with a homing device — to deliver a potent cancer-killing payload only to glioblastoma cells.