Glioblastoma (GBM) is known as one of the most common, complex, treatment-resistant, and deadliest cancers. These tumors devastate the brain, which controls cognition, mood, behavior, and personality, as well as every function of each organ and body part. The current standard of care can only prolong a patient’s life by a few months, on average, but it can also drastically reduce their quality of life.
Let’s talk about some of the lesser-known challenges that people living with glioblastoma and their caregivers face.
Seizures
Seizures are a common symptom in patients with brain tumors, including GBM.
“He had a small seizure, and then on the way to the hospital where an ambulance took him, he had several grand mal seizures,” explained Katie M., whose husband has glioblastoma. “Like many other patients with brain tumors, you don’t know something’s wrong until all of a sudden a seizure hits.”
Seizures can contribute to cognitive issues, affecting memory, attention, and executive function. In addition to the physical difficulties associated with seizures, including fatigue, other aspects can prove challenging.
Loss of Independence and Social Isolation
Seizures can disrupt daily activities and routines, making it difficult to maintain independence. Not only that, but many states require drivers to be seizure-free for some time before they can legally drive again. (The Epilepsy Foundation provides driving laws by state.) This requirement means an unforeseen seizure can immediately create a loss of independence by taking away one’s ability to drive and leaving the patient entirely reliant on others for transportation.
Additionally, patients may avoid certain social situations — like a big, public event away from home — due to their concern about having a seizure in public. This worry can lead to social withdrawal and isolation, as they second guess whether they can accept invitations to social gatherings — big and small.
Experiencing Anti-Seizure Medication Side Effects
Keppra (levetiracetam) is a commonly prescribed antiepileptic drug used to control seizures. While it is generally well-tolerated, some patients experience significant behavioral side effects, one of which is colloquially known as “Keppra rage.” Side effects can range from mild irritability to severe aggression and emotional instability.
Patients living with glioblastoma are already at an increased risk of anxiety and depression due to the emotional burden of their diagnosis and the impact of the tumor itself. Keppra rage can exacerbate these conditions, making emotional management more difficult.
It means some patients with GBM may have to navigate trying to minimize seizures with medication and their overall mental health under the guidance of their health care team.
Other common Keppra side effects include fatigue, weakness, dizziness, headache, and drowsiness. It’s important for patients to talk to their health care team about any side effects they may experience.
Balance and Falls
Glioblastoma can significantly impact a patient’s balance, increasing their risk of falls. Their imbalance can arise from the tumor’s location, seizures, surgery, treatment, or even medication side effects.
An article in the Neuro-Oncology Practice reports that “more than 70% of patients with malignant glioma report motor dysfunction as a problem at some time during the disease course.”
It’s important for people living with GBM and their care partners to monitor and then promptly address balance issues, perhaps through assistive devices, to ensure safety and improve their quality of life.
According to Dr. Eric Galvez, a former therapist turned patient and advocate, “Falls can be devastating to oncology patients with unexpected emergency room visits, fractures, or even [long-term] hospital admissions.”
Fear of Recurrence
Fear of cancer recurrence is a common experience for people living with brain tumors, particularly for patients with glioblastoma. According to an article in the Journal of Clinical Oncology, “most GBM recurs in 6-9 months.”
This fear may affect one’s quality of life, as it can have profound psychological, emotional, and practical impacts on oneself and their support network.
Taylor G., who has glioblastoma, explains, “Occasionally, it’s hard to keep the thoughts out of your mind like, ‘What if it comes back?’ I just try not to think about it and stay busy. When they find something unsettling on a scan, I try to put all my effort and focus into either my woodworking business or watching my kids do gymnastics or jazz dance. If I don’t have anything I’m working on, I’ll just go out and start cutting wood because it’s a good stress reliever.”
Scanxiety
Fear of recurrence can also contribute to scanxiety, which is the stress and anxiety one feels before, during, and/or after medical imaging.
“A scan is a determination of what’s happened and what I have to do next,” said Ann S., who had an MRI every two months to look for any regrowth after being diagnosed with GBM. “I think it’s very high anxiety-producing because it basically decides whether the last two months of chemotherapy have been working. The scan is highly decisive about my quality of life.”
For patients struggling with scanxiety, there are actions they can take to cope with scan-related anxiety, including self-care.
Memory Loss
“When a person has a brain tumor, it can affect their cognition, which is memory, executive functioning, ability to understand what somebody’s saying, and ability to express what you’re saying,” said Mary Lovely, PhD, NBTS’s former patient navigator. “When your cognitive abilities have been affected, your whole life changes.”
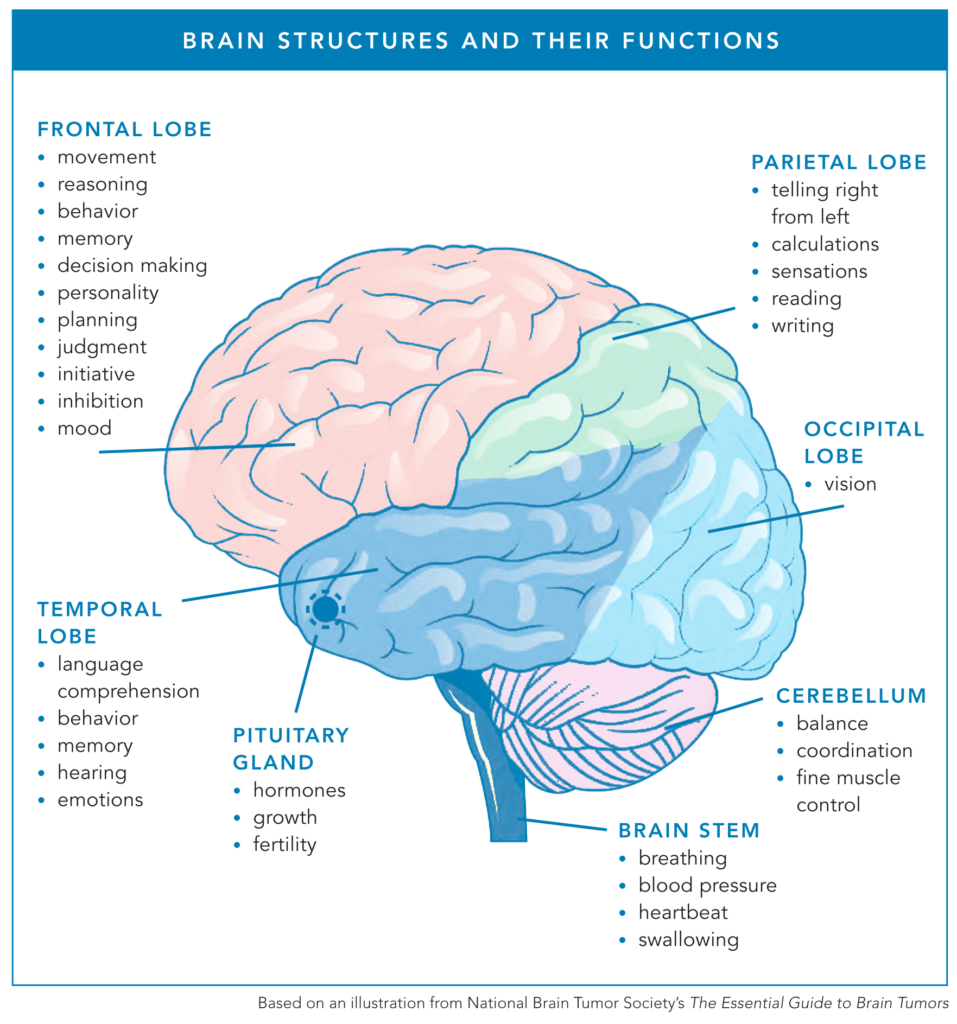
Glioblastoma is most commonly found in the frontal and temporal lobes, although GBM can certainly arise elsewhere in the brain. Both the frontal lobe and temporal lobe are responsible for memory, so a tumor in either location can affect one’s ability to store or recall memories.
Memory problems can make routine tasks challenging. For example, a patient may forget to take medications at the right time or dosage, lose track of schedules, or even accidentally leave the stove on.
“My biggest issue is my memory,” said Taylor G. “Short-term memory is a problem.”
Memory aids such as calendars, alarms, and written reminders can help manage daily tasks and reduce reliance on memory.
“Often with recurrence, we see short-term memory issues as well as just feeling foggy or loss of continuation of thoughts,” said Katherine Pahler, RN, NBTS’s patient navigator. “It’s important to let patients know that this isn’t uncommon, and there are resources to help.”
Cognitive rehabilitation therapy, for example, can help patients develop strategies to cope with memory deficits and improve cognitive function.
Fatigue
Fatigue is a common and debilitating symptom for people living with GBM. This overwhelming sense of tiredness can significantly affect various aspects of a patient’s life, from daily functioning to emotional well-being.
A Neuro-Oncology Advances article highlights that “48% of glioblastoma patients report fatigue after surgery, and this number increases to up to 90% in patients with tumor recurrence.”
People living with glioblastoma can face both physical and cognitive fatigue, resulting in reduced energy levels and mental exhaustion.
“Fatigue has been the hardest for me out of all of the symptoms because I feel like fatigue takes away from my quality of life,” said Tresa Roebuck-Spencer, PhD, a neuropsychologist living with glioblastoma. “It makes it where I feel hesitant to go out because I never know when that fatigue is going to become too much.”
Lack of Treatment Options for Recurrence
Currently, there is no uniform standard of care for recurrent glioblastoma, which means it’s up to the patient and their health care team to determine their next steps.
One of the challenges patients with GBM recurrence can face is that they have already undergone a variety of treatments to get to that point, which may exclude them from clinical trial opportunities.
“It’s unfortunate that there’s so many exclusion criteria to participate in these trials and many of them are based on past treatment,” Tresa explained. “There were some treatments I tried to put off having — like Avastin — because I knew that once I got Avastin, it would exclude me from future trials. I tried not to take that treatment for as long as I could.”
Tresa recently spoke with her doctor about these frustrations saying, “You don’t get to 3.5 years without having gone through a lot of treatments and, unfortunately, these treatments exclude you from future trials.”
Financial Challenges
Not only do patients and their caregivers have to navigate the physical and emotional ramifications of a GBM diagnosis, but they must do so while managing the high costs of surgery, treatment, therapies, and more.
Glioblastoma is one of the more expensive cancers to treat, often leaving patients and families with major financial hardship on top of the burdens of the disease. One study found “the direct medical costs of newly-diagnosed, TMZ-treated GBM in commercially insured patients” to be “substantial with estimated total cumulative costs of $268,031.”
“Even with a great steady income and decent savings, this is a really expensive, life-changing financial situation that is really difficult to plan for,” shared Katie M., whose husband has GBM. “I think the threshold for where financial toxicity begins needs to be put a little higher to match the gravity of the situation.”
NBTS has a list of financial assistance resources available to patients living with brain tumors.
Last Updated: June 16, 2025