The highlighted portion of Dr. Sawyers quote speaks to how tumor cells are able to adapt, and use different mechanisms than they were originally using to continue growing. Thus, the drug that was being given as a treatment – which had specifically been designed to target and inhibit the original mechanism – is no longer effective. This, is why some cancer drugs stop working in some patients.
While, drug resistance is a challenge for all tumors and cancer, it is especially difficult for very aggressive and complex tumors like many malignant brain tumors.
One of the possible prescriptions Dr. Sawyers notes for overcoming the resistance problem in cancer, is for researchers from across the country to work together and share their data and knowledge to help understand how tumor cells develop resistance.
This was part of the rationale that the National Brain Tumor Society had in mind when we developed the Defeat GBM Research Collaborative.
Defeating Resistance in GBM
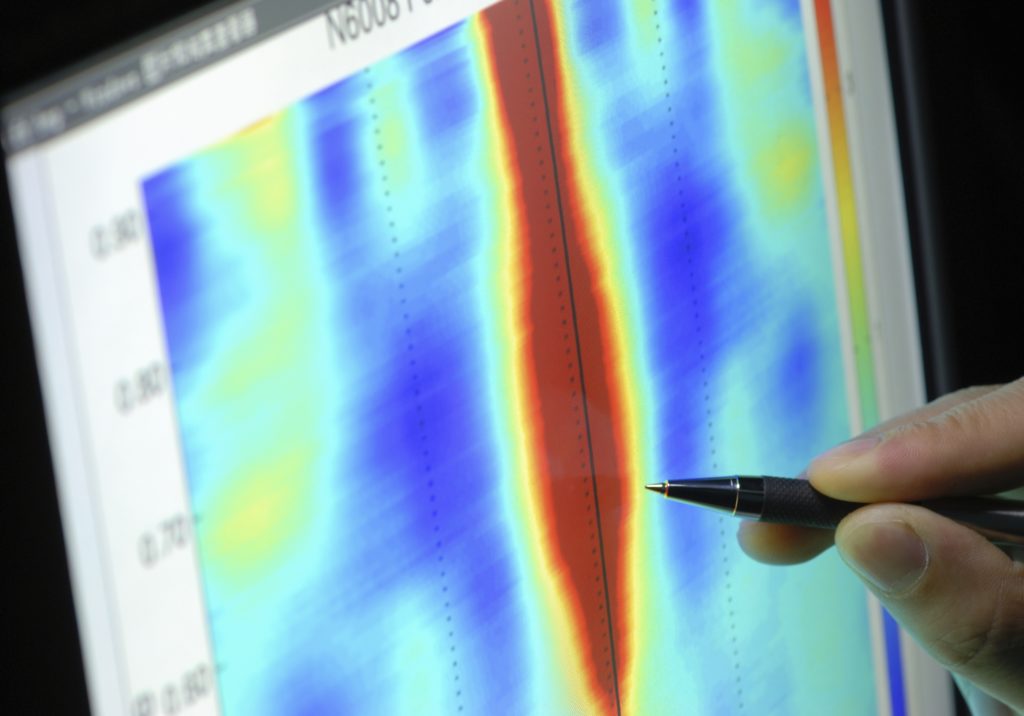
One of Defeat GBM’s four complementary projects, the Discovery effort – led by Ludwig Cancer Research scientists Dr. Webster Cavenee and Dr. Frank Furnari – aims, specifically, to identify and target the ‘escape and evade’ methods GBM cells use to develop resistance.
The scientists working in the Defeat GBM Research Collaborative held one of their regular check-in calls earlier in April, and it was the Discovery team from Ludwig’s turn to give the full group an overview on their current progress.
The Ludwig team is targeting EGFR, as well as other well-characterized GBM mutations. Their goal is to find out after they inhibit targets like EFGR (which is over-expressed in many GBM tumors), what new mutations the tumor cells use to continue growing. Once these so-called resistance mechanisms are known, a combination therapy could be used both inhibit the tumors initial mutations, as well as its subsequent escape route.
One of the National Brain Tumor Society’s Strategic Scientific Advisors, Dr. Anna Barker, is a co-director of a program at Arizona State University called the “Complex Adaptive Systems Initiative.” This is a perfect name for the study of many cancers, like malignant brain tumors. Tumor cells are not just complex, but they also are able to adapt and use a system of interrelated pathways to continue to grow even as today’s best medicines are being applied.
We hope for a future where a combination of new, or existing, drugs can be identified and utilized to overcome resistance. And Programs like our Defeat GBM Research Collaborative aim to do just that.