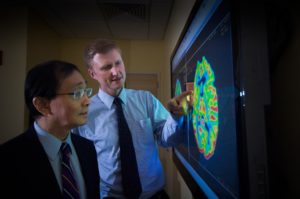
Cover photo courtesy of the website of the National Cancer Institute
When an athlete injures their knee, ankle, shoulder, etc. they will often need to go for an “MRI” to determine the extent of the damage done to the affected area. And in most cases the MRI will be able to diagnose the issues with relative ease, accuracy and expediency.
Most Americans are familiar with MRIs – which stand for “magnetic resonance imaging” – and their effectiveness as a technique for doctors to capture an image that is used to interpret an injury. And most in the brain tumor community know from experience that MRIs play a critical role in diagnosing and determining whether a patient’s brain tumor is responding to treatment.
But what may come as a shock to some is that there is a lack of confidence in the use of MRIs in brain tumor clinical trials – when potential new drugs are being tested – to determine whether patients are actually getting benefit from the investigational therapy.
This is because there have been issues with variability in terms of how MRI machines are used at different treatment centers and in the interpretation of tumor measurements made by the professionals that read the MRI images. This lack of standards in MR imaging acquisition protocols, along with differences in MR scanners themselves (i.e. field strength, gradient system, manufacturer sequences), has limited the ability to combine imaging data across sites in a multi-center clinical trial.
As you can imagine, this constitutes a significant problem when it comes time to evaluate the effectiveness of the drug that was being tested – and ultimately can impact the FDA’s ability to determine if a new drug is working against a brain tumor.
Measuring the benefits of a treatment to a patient – known as “endpoints” – so that the U.S. Food and Drug Administration (FDA) can be confident enough to approve that a drug is working is one of the major challenges in developing new treatments for brain cancer.
If researchers and companies conducting brain tumor clinical trials can’t rely on images from MRIs to determine if a drug is having an impact against patients’ tumors (or “imaging endpoints”), then the only way they can tell if a potential new treatment is working is by survival data. However, using survival data to evaluate a potential new treatment (which typically necessitates using an endpoint known as “Overall Survival”) routinely requires clinical trials that are longer, more expensive to run, and need more patients than trials that use imaging-based endpoints.
This is why the National Brain Tumor Society formed the Jumpstarting Brain Tumor Drug Development Coalition in 2014, as part of our Clinical Trial Endpoints Initiative. The Coalition then hosted a workshop with key parties from the FDA, NCI, nonprofit research institutions, companies, advocacy organizations and other experts focused specifically on the use of imaging-based endpoints in brain tumor clinical trials.
An outcome of this workshop was the determination that a steering committee needed to be established to develop new recommendations for a standardized protocol for how MRI images are to be captured during clinical trials that include patients from multiple treatment centers.
Now, I’m happy to reveal that the steering committee has just published a paper on its work, which announced new, consensus recommendations for a standardized “Brain Tumor Imaging Protocol (BTIP),” which will improve the accuracy of imaging data in brain tumor clinical trials and help to better assess if a new treatment is effective.
Standardization will reduce variability and help validate, and build confidence in, the use of imaging-based endpoints for drugs seeking FDA approval. In turn, the use of imaging endpoints will help enable researchers and companies to hopefully shave off the time it takes to ultimately get a new treatment approved. This will, in turn, help “jumpstart” a new pipeline of treatments that can ultimately benefit patients.
Beyond its promise to ultimately deliver more treatment options to patients (and faster), the new Brain Tumor Imaging Protocol represents the power of patient advocacy, as well as collaboration. Led by the National Brain Tumor Society, a Coalition of nonprofit groups was able to bring the entire brain tumor field together to achieve a new process that will help improve the speed and volume of future brain tumor drug approvals.
The BTIP is also an example of the National Brain Tumor Society’s efforts to create systemic change and our ability to achieve positive outcomes as a leader and objective facilitator in this field. The BTIP is changing the way clinical trials for new brain tumor drugs can be conducted by opening up new accelerated pathways for evaluation and approval. The cumulative results from this will ultimately save time, money, and hopefully lives.
As always, we could not have taken on this effort without community support. As such, I would like to take this opportunity to again thank all of our Coalition partners – Accelerate Brain Cancer Cure, The Musella Foundation, and the Society for Neuro-Oncology – as well as the many companies, researchers, patients, doctors, FDA and NCI leaders who participated in the conversations that led to the publishing of this protocol. And last, but certainly not least, all of our donors, advocates, and volunteers who drive us to fight for the brain tumor community each and every day.
Sincerely,
David Arons