As part of our effort to raise awareness during Childhood Cancer Awareness Month, we created an infographic about our newest initiative that aims to get new and better treatments to children with brain tumors: Project Impact.
Today, we want to spend some time talking about a major piece of that initiative, the so-called “preclinical testing platform.” This is represented in the infographic as a “lack of testing models that adequately predict drug response in children,” and that we are trying to change this with “data-driven models.”
So what does that all really mean? Why is it so important?
We’ve talked a little about the problem (in the seventh paragraph in this previous blog, and also in the seventh paragraph of the press release), before, but here we hope to step back and take a deeper dive.
What is a preclinical testing model?
Before a new medicine or treatment becomes available for any cancer, it must first go through the clinical trial process. The clinical trial process is when potential new therapies seeking approval are first tested in sample groups of patients to ensure they are adequately safe and effective before being made available to an entire population.
However, before a potential new medicine or treatment can even enter the clinical trial process, it must first show promise in what is called the “preclinical” setting – hence the name (pre – before – the clinical trial process!).
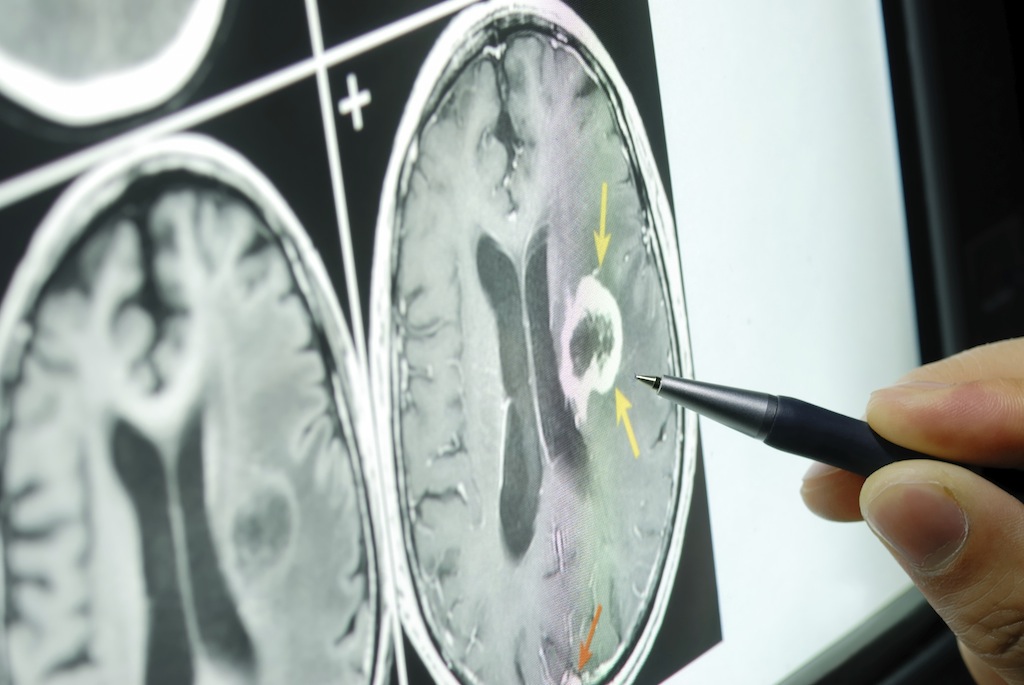
In order for a cancer treatment to show promise in the preclinical setting it must be run through a number of tests. Among other things, these tests seek to determine if the medicine is getting to the tumor cell; getting there in a high-enough dose to create an effect on the tumor; doing so while harming as few healthy cells as possible; and, ultimately, whether the tumor cells stop growing and/or die.
These tests typically take part using real tumor tissue that has been obtained from patient biopsy and been engineered into a “cell line” or “cell culture” (think a petri-dish or test tube in your middle or high school biology class). These experiments in tumor cells are often referred to as in vitro (“within the glass” or “outside the body”) testing.
Typically, if in vitro testing for a potential new treatment is promising it will move on to the next step in preclinical testing, which is testing in animals (typically mice), called in vivo (“within the living” or “in the body”).
In cancer research, the goal is to make preclinical testing in cells and animals produce information (data) on how the potential new treatment interacts with a tumor in order to predict as accurately as possible what might happen if that medicine was given to a human patient with a brain tumor. So in that light, the cells and animals that are used to test these drugs in the preclinical setting are modeled as closely as possible to a tumor in a human. Hence the term preclinical testing models.
The preclinical testing platform refers to all of the different cell lines, animal models, and list of tests that will need to be performed on a potential new treatment undergoing evaluation. So for example, a preclinical testing platform might consist of, say, two different types of animal models, with 10 animals in each model, 5 different cells lines, and 6 different tests to perform on each of them.
However, we know that tumor cells outside the body and in mice both often act differently than tumors do in humans. Which brings us to the next important question…
What is the trouble with current preclinical testing models?